

African Journal of Respiratory Medicine received 855 citations as per google scholar report
Case Report - (2025) Volume 20, Issue 1
Received: 04-May-2025, Manuscript No. ajrm-25-165146; Editor assigned: 06-May-2025, Pre QC No. ajrm-25-165146 (PQ); Reviewed: 20-May-2025, QC No. ajrm-25-165146; Revised: 04-Jul-2025, Manuscript No. ajrm-25-165146 (R); Published: 11-Jul-2025, DOI: 10.54931/1747-5597.25.20.61
Lymphomatoid granulomatosis is a rare Epstein Barr virus-driven B cell lymphoproliferative disease. It is a distinctive type of malignant lymphoma associated commonly with immunosuppression. The lungs are the most commonly involved organs. We present a case report of a 45-year-old immunocompetent gentleman who was diagnosed with pulmonary lymphomatoid granulomatosis. He presented with symptoms of an upper respiratory tract infection and persistent fever. His Biofire Adenovirus PCR test on the throat swab was positive with a normal Chest X-ray and CRP 47 and PCT 0.17. His clinical condition deteriorated despite treatment with Tamiflu for four days and he developed respiratory distress, hypoxaemia and septic shock. Bronchoscopy and lavage results showed Adenovirus infection only, normal cytology and negative for fungi and bacteria. A lung biopsy confirmed the diagnosis of lymphomatoid granulomatosis, he was treated for EBV with Gancyclovir with good clinical response and referred to an Oncologist.
Ebstein-Barr virus; Information technology; Perfalgan; Tamiflu; IV fluids
Lymphomatoid granulomatosis is a rare Ebstein-Barr Virus (EBV) driven disease. It’s a malignant lymphoma which is diagnosed histologically and divided into 3 grades histologically depending on the density of EBV infected cells. Although rare, this case highlights the fact that diseases can present atypically (immune competent individual presenting with this condition as well as Adenovirus and EBV co-infection in a patient with lymphomatoid granulomatosis [1-5].
This is a case of a 45 year old gentleman, IT( Information Technology) specialist and professional cyclist who had been previously well. He presented to hospital with a 3 day history of fever, sore throat, myalgia and loss of appetite. He denied having cough, shortness of breath or chest pains. Of note, his daughter had been having flu like symptoms and a bout of diaarhoea over the past week prior to his admission.
The patient’s presentation of fever, sore throat, myalgia, and loss of appetite, alongside a recent exposure to flu like symptoms from his daughter, raised concern for a viral etiology. immunocompetent Although typically individuals, rare in lymphomatoid granulomatosis, driven by Epstein-Barr Virus (EBV), was considered in light of his systemic symptoms. Further investigation revealed co-infection with Adenovirus and EBV, a combination that added complexity to the diagnosis. His history as a professional cyclist and IT specialist, with no prior significant medical issues, underscores the unpredictable nature of EBV-related malignancies, reinforcing the need for a thorough and timely investigation in atypical presentations [6-10].
Clinically, on admission, he was comfortable in room air. He had a pyrexia of 39C, tachycardia of 118 b/min and he was normotensive. Respiratory exam was otherwise unremarkable and on ENT exam, he had a pharyngitis. The rest of the systemic examination was normal.
A septic screen was done, including throat swabs for SARS-2-CoV, and respiratory viruses PCR panel (Respiratory biofire). The throat swab result came back positive for Adenovirus. His renal function was normal, full blood count was normal and his CRP was 47. He was commenced on IV Perfalgan, Tamiflu, IV fluids.
Over the next 2 days, his temperatures were still spiking despite the IV paracetamol and voltaren supp. On the fourth day, his condition deteriorated-he went into respiratory distress: With a tachypnoea of 32 bpm, became hypoxic and he went into septic shock. A septic screen was repeated, IV fluid resuscitation was done, with crystalloids and antibiotics were escalated. A CTPA (CT Pulmonary Angiogram) was done which showed no pulmonary embolus, however pulmonary nodules as well as hilar lymphadenopathy, dense consolidation on the left lower lobe was seen. A repeat SARS-Cov-2 PCR swab was done, which came back negative. The patient had developed renal impairment, with the eGFR now having dropped to 36 ml/kg/hr, his CRP was now 249.6, PCT of 1.99, platelet count was 137 and he had developed a lymphopaenia of 0.73. Over the next 4 days the patient stabilized haemodynamicallly, was still oxygen dependent and his inflammatory markers had come down. He had a Bronchospcopy and Lavage (BAL)done, the results of which still came back positive for Adenovirus, microscopy and culture revealed C. auris, which was sensitive to Fluconazole [11-13].
After 3 days, seeing that he had not settled completely on IV antibiotics and Fluconazole: He had a lung biopsy done, which showed features of Lymphomatoid granulomatosis:
• Bronchi and lung tissue: Dense lymphohistiocytic and plasma cell infiltrate surrounding the areas of coagulative and haemorrhagic necrosis. EBV positive cells.
• Rest of lung tissue: multiple large cells with nuclear and cytoplasmic inclusions: PCR testing confirmed Adenovirus infection.
• Angiitis: Arteries demonstrated mural oedema and lymphocytic infiltrate.
• In multiple fields: Capillaries demonstrated fibrin thrombi, small foci of granulation tissue within the alveolar spaces (Figures 1-3).
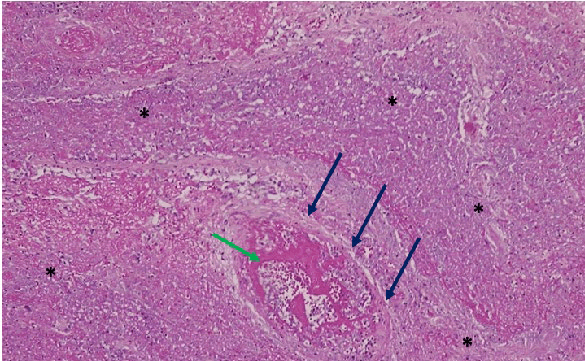
Figure 1: Lung tissue showing haemorrhagic and liquefactive necrosis (*). Blood vessel (blue arrow) shows central thrombus (green arrow).
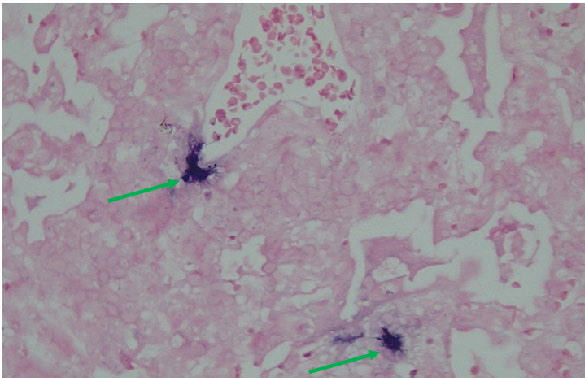
Figure 2: EBV positive cells (insitu hybridization studies) [green arrow].
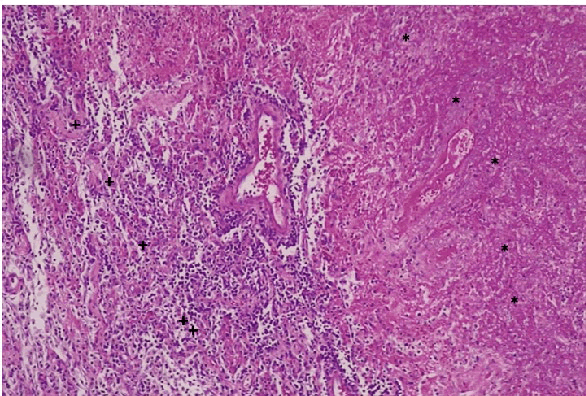
Figure 3: Coagulative necrosis (*) bordered by lymphohistocytic inflammation (+).
Based on the histology, he was diagnosed as having grade 2 pulmonary lymphomatoid granulomatosis and hence he did not require chemotherapy. He was commenced on IV Gancyclovir which he responded very well to, IV steroids and we continued the Fluconazole. He was discharged on oral Valgancyclovir for 14 days as well oral Fluconazole.
Lymphomatoid granulomatosis almost always involves the lungs where it usually presents as bilateral pulmonary infiltrates- other common extra-nodal sites, including skin, central nervous system, liver and kidneys. The atypical lymphoid cells directly accumulate within affected tissues and clinically present in the form of infiltrative lesions.
The diagnosis of lymphomatoid lymphomatosis is based on the histological triad comprising the following:
• Nodular polymorphic lymphoid infiltrate composed of small lymphocytes, plasma cells and variable numbers of large atypical mononuclear cells. • Angiitis due to transmural infiltration of arteries and veins by lymphocytes (a process distinct from vasculitis in which acute and chronic inflammatory cells are found with associated vessel wall necrosis).
• Granulomatosis (central necrosis within the lymphoid nodules and not granuloma formation).
Pathologically, it is graded by the number and density of EBV+ atypical B cells. What is striking in this patient is that:
• Adenovirus and EBV co-infection is unusual in patients with lymphomatoid granulomatosis and the authors did not come across any case reports with this condition.
• It is not clear exactly, as to what role the Adenovirus played in the case-whether it triggered and hence unmasked the lymphomatoid granulomatosis or it was just an innocent by-stander. The fact that it was picked up on the PCR test (throat swab), broncho alveolar fluid and the lung tissue seems to suggest that this was quite a severe infection and the patient was able to mount a vigorous immune response.
• LYG is rare in immunocompetent hosts, our patient was young and fit, HIV negative, normal Immunoglobulin levels and yet he developed this rare condition. It raises the concern of whether he had underlying Inborn error of immunity or mutations in T and B cell signalling. Inborn errors of immunity are a heterogenous group of about 450 genetic disorders predisposing to severe/recurrent infections, autoimmunity or development of severe/early onset neoplasia or lymphoproliferation. Monogenic disorders of T and B cell signalling predispose to lymphoproliferative disorders caused by EBV. Due to unavailability of resources and infrastructure, these genetic tests are not done locally, however, we would have loved to test him to see if he indeed does have any of these mutations which predisposed him to develop this condition.
The phrase "needle in a haystack" symbolizes the daunting and often futile search for something elusive in a sea of complexity. In life, we often find ourselves overwhelmed by challenges that seem impossible to overcome or truths that are buried deep beneath layers of confusion. However, this metaphor also underscores the importance of persistence, patience, and determination. While the search may appear endless, it reminds us that the effort itself can lead to personal growth, and sometimes, the most valuable discoveries are found in the most unexpected places. Ultimately, it’s the journey, not just the destination, that counts.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Select your language of interest to view the total content in your interested language
To read the issue click on a cover